Describe the features of a flail chest.
Answer:
Flail chest is when there is a free segment of the thoracic wall. This usually means 3 or more ribs broken at 2 points causing the segment to lose bony continuity with the rest of the chest wall.
Question:
How much bloods loss can be anticipated from a rib fracture?
Answer:
Up to 150mls of blood loss from rib fractures.
Question:
What are the implications of a flail segment?
Answer:
There are 4 main implications of a flail segment.
1. The inability to generate adequate negative intrathoracic pressure for inspiration due to the free segment can cause respiratory fatigue and subsequently Type II respiratory failure. This is a failure of ventilation, not of oxygen transfer therefore the patient will have hypercapnia.
2. Presence of a flail segment is indicative of high impact forces. As the chest wall is relatively pliable, a large amount of force is required to cause rib fractures. Such high forces may indicate the presence of other injuries.
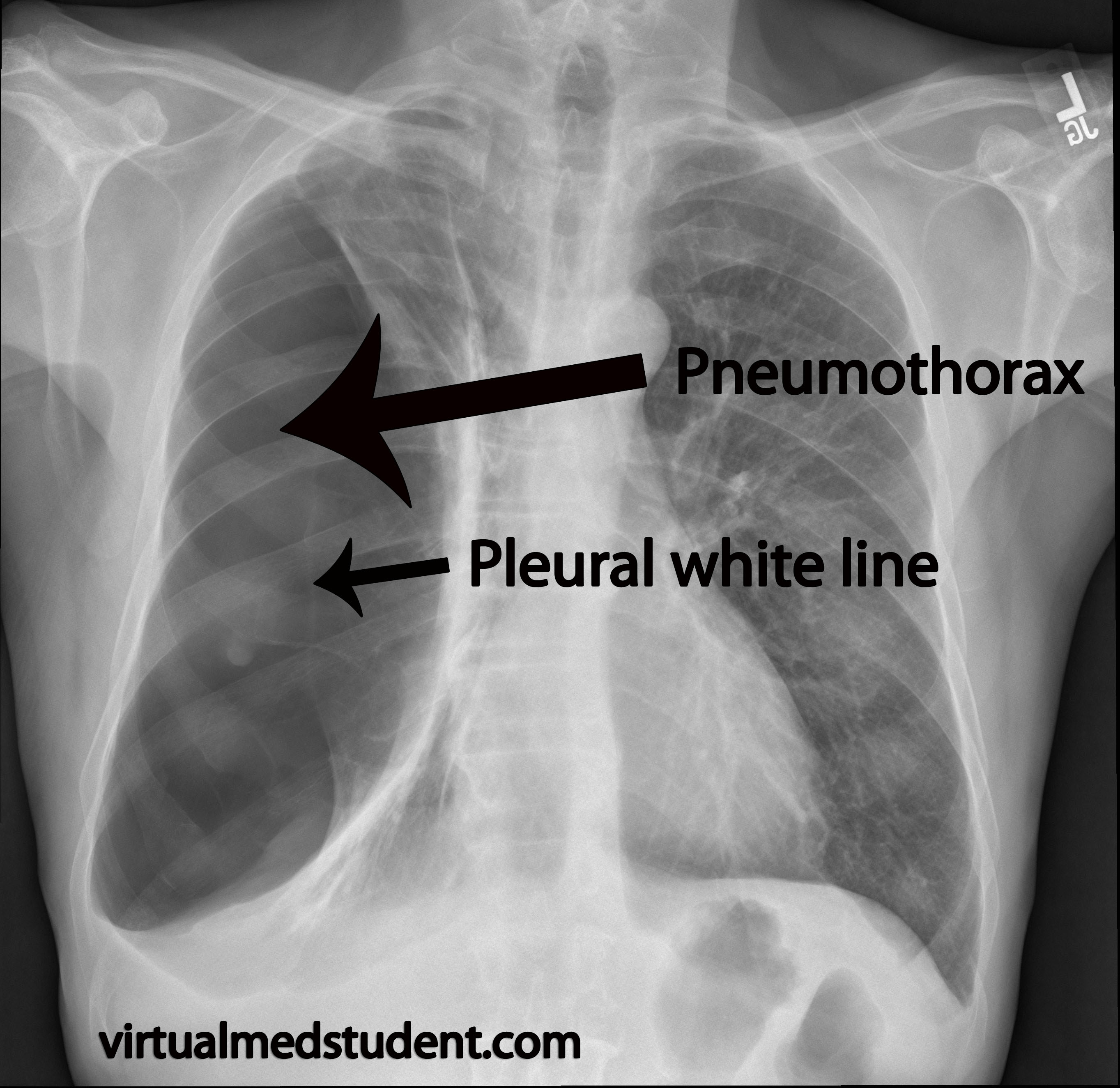
3. There may be other underlying injuries. Haemothorax, pneumothorax, pulmonary contusions, diaphragmatic ruptures and cardiac trauma, including cardiac tamponade, are all possible concurrent diagnoses.
4. Infection and pneumonia in later stages is also a complication due to the inability to ventilate the lower lobes of bilateral lungs due to pain, or due to cardiac contusions.